STS-58 Payload Commander Rhea Seddon spins the Spacelab Life Sciences rotating chair as Payload Specialist Martin Fettman serves as a test subject during a medical research mission in 1993.
Photo Credit: NASA
NASA Chief Health and Medical Officer James Polk shares lessons learned about the human element of spaceflight.
Editor’s Note: NASA’s Office of the Chief Engineer and the Human Exploration and Operations Mission Directorate sponsored the Human Spaceflight Knowledge Sharing Forum in November 2016. Select individuals responsible for shaping NASA’s future over the next 10 to 20 years focused on technical best practices and lessons learned from successful and unsuccessful human spaceflight missions. This is part of a series of articles recapping lessons learned and knowledge shared by these individuals at the pilot knowledge sharing event.
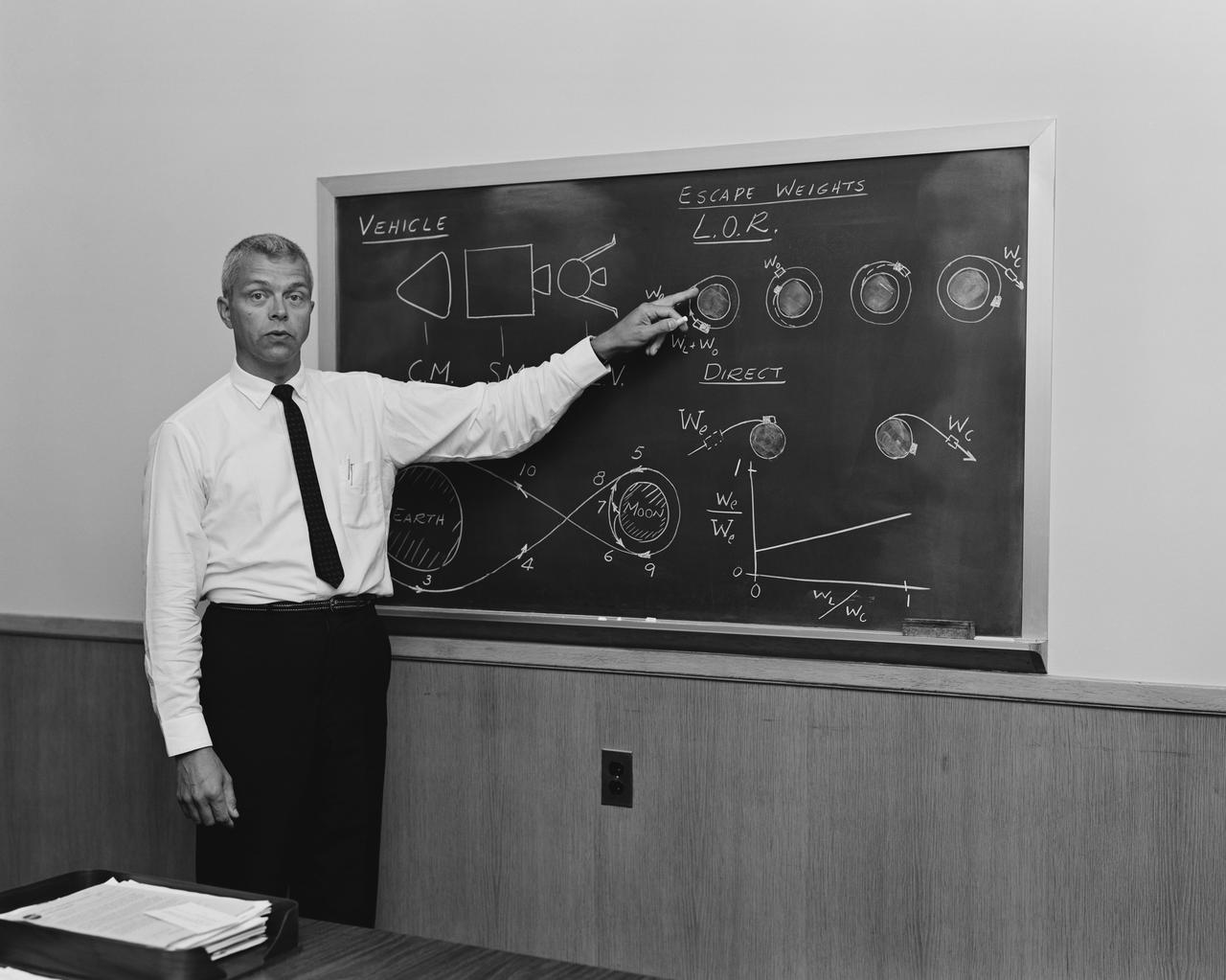
“The human system is the only system in engineering that you can’t take to failure,” said NASA Chief Health and Medical Officer James Polk, D.O., at NASA’s recent Human Spaceflight Knowledge Sharing Forum.
“I am horribly jealous of the folks in engineering who can take a part and stress it and break it, and take 50 parts and get little dots on a graph to figure out where that part breaks,” said Dr. Polk. “I can’t do that to [Astronaut] Kjell Lindgren. I can’t take him and see where he breaks or where he fails. It’s generally frowned upon to do that on a human system.”
Dr. J.D. PolkPhoto Credit: NASA/Joel Kowsky
Polk spoke candidly about the tension between the medical and engineering communities when defining requirements for space missions. “You guys hate it when I say, ‘It depends,’ because you want a firm number or requirement. I’ve had engineers say, ‘It looks like this in the textbook.’ Well, that’s not what it looks like when you’re actually doing the surgery,” he said.
He addressed some of the differences between how doctors and engineers think. “You design your systems. We actually have to reverse engineer nature to understand the system,” said Polk. “You use quality-controlled components. There isn’t anything quality-controlled about the human body. You use established frameworks and employ physical laws, and we have to discover the concepts in qualitative relationships as we go.”
Polk’s passion and compassion came through as he recounted the unenviable responsibility of dealing with tragic loss of life when accidents occur. “In meetings, when folks start to talk about graphs and lines and loss of crew, we will purposely inject somebody’s name into the discussion just to make sure that folks realize what’s at risk here. I try to put a face on this,” he said. “At the end of the day, my job is to make sure the astronaut survives.”
Polk is responsible for the oversight of health and medical activities at NASA, including medical aspects of all national and international NASA missions involving humans. He led a forum session on “Human Factors/Human-Centered Design: What Did We Think and Do?” and shared his experiences and perspectives on human factors and medical lessons learned from decades of human spaceflight data and research.
Physiologic Challenges
The human body always tries to reach homeostasis, an equilibrium with its environment, which is hard in microgravity. Polk said a lot of medical lessons were learned through Mercury, Gemini, Apollo and the Space Shuttle Program, but the International Space Station (ISS) presented totally different physiologic challenges that occurred as a result of increased time in microgravity.
A new understanding of Visual Impairment and Intracranial Pressure (VIIP) is one of the biggest lessons learned through medical evaluation of ISS crew members. About 40 percent of the astronauts who spend a couple of months on ISS complain of vision change. Through 3 Tesla MRI and other diagnostic test results, Polk and his medical colleagues at NASA observed changes in the optic nerve that goes from the brain to the eye, and a flattening in the back of the eye along with choroidal folds — similar to wrinkled carpet — in the back of the retina. The medical doctors initially thought the problem was caused by fluid changes that occur on orbit, but then realized the vision problems sometimes linger several years after spaceflight. NASA has initiated clinical and research protocols to acquire and analyze data on all astronauts to define the exact origin of the potentially harmful vision changes and is seeking possible preventive measures.
Polk also shared lessons learned about Space Adaptation Syndrome, formerly called Space Motion Sickness, which he says has “absolutely nothing to do with motion.” In the early days of spaceflight when the vomiting, queasiness, disorientation and headaches were thought to be motion-related, the prevailing assumption was that astronauts could be conditioned by spinning in a centrifuge in preparation for spaceflight. But they still got sick.
Polk explained why approximately 78 percent of astronauts get Space Adaptation Syndrome. “You have about 112 signals that come up to your brain that tell you where you are at any moment in time to allow you to walk or ride a bicycle, etc., and stay upright. But after eight minutes of spaceflight, in the most exciting ride of your life, you get up. Your partner is upside down, so your eyes say, ‘Wait a minute. That’s not right. Your semicircular canals, which have fluid in them, now are floating. The fluid is floating and it’s not moving around in the same direction that it did on Earth. You don’t have any pressure on the balls of your feet or your heels because you’re floating. You don’t have any pressure on your rear end because you’re no longer sitting on your seat. Your Golgi tendon apparatus doesn’t have the stretch on it,” Polk said. “All of a sudden, 112 confusing signals come to your brain, and your brain says, ‘I don’t know what just happened, but I’m going to throw up.’” He said fewer incidents of the syndrome occur with capsules — such as Mercury, Gemini and the planned Orion crew vehicle — than on space shuttle and ISS because the brain is deciphering fewer mismatched cues, such as an astronaut upside down.
Space Medicine Challenges
Among the unique challenges of space medicine is research. “Normally, when we do research in medicine, we’ll do something at the Cleveland Clinic or similar institution with about 2,000 patients and we can get a really good “n” number,” said Polk. “With space medicine, unfortunately, one is a control, two is a series, and three is a prospective randomized trial.”
Another challenge has been long-term health care for crew members. Space travelers are at higher risk for radiation-induced cancer, bone loss and fractures, and a variety of health issues. Polk’s predecessor, Richard Williams, M.D., has been a longtime proponent of legislation to provide lifetime comprehensive health care for former astronauts. In March 2017, Congress passed and the president signed the To Research, Evaluate, Assess, and Treat Astronauts Act, also known as the TREAT Astronauts Act, as part of the NASA Transition Authorization Act of 2017 – allowing NASA to treat former astronauts for medical issues that may have resulted from spaceflight.
| Related Video: Dr. Richard Williams on Comprehensive Health Care for Crew |
Medical Risks
Radiation risks during long-duration spaceflight garner a lot of media attention, but Polk says he’s more concerned about long-term risks of radiation than immediate effects during the mission. In fact, he said this is where the mindset between physicians and engineers differs the most because the mission is over for engineers when the wheels stop. For physicians, the mission continues for the remainder of the astronaut’s life as they monitor health conditions that could be related to spaceflight.
During his forum presentation, Polk emphasized the importance of human system integration and said it has to be improved. “We’ve seen in multiple different areas where human factors were ignored. What we typically do is look at the spaceflight environment, try to reduce the hazards, look at the evidence base in medicine, and through the Human Research Program try to reduce those risks to try to implement standards and requirements and then mitigate them for any remaining risk that comes on,” he said.
It shouldn’t be an easy conversation, according to Polk, who resolutely explains medical risk to program managers. “We should cuss and discuss and get heated in arguments because the risk is really high on the other side if we screw this up. And I don’t want that to be an easy, amiable, ‘love you, man’ conversation. It’s supposed to be hard,” he said. “I want the program manager to be awake at 2 o’clock in the morning thinking about whether or not this was the right decision. There are some risk trades and some very difficult discussions to have. It’s not going to be easy, and it’s not supposed to be.”
Related Videos:
| Richard Williams, M.D., on Risk Acceptance in Health and Medical | Richard Williams, M.D., on Health and Medical Requirements |